NEWS RELEASE
OFFICE OF ATTORNEY GENERAL
*************************
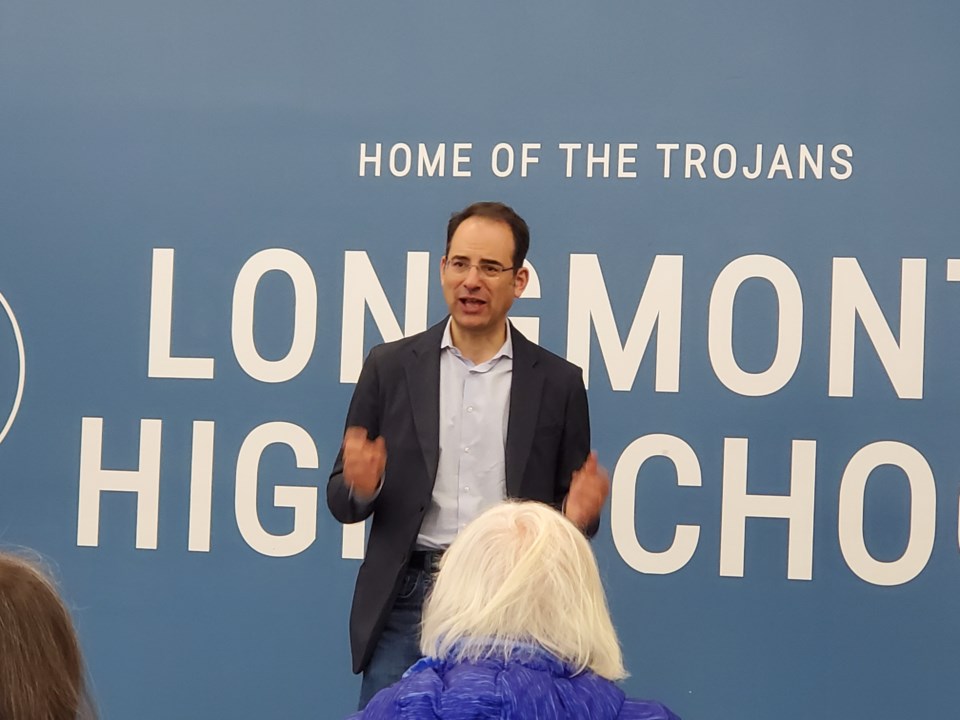
DENVER -- Attorney General Phil Weiser today joined a bipartisan coalition of 38 other attorneys general urging Congress to reform the way pharmacy benefit managers, or PBMs, conduct business and bring more transparency to their industry.
“With too many people struggling to afford basic needs like medicine, it’s unconscionable that a small but powerful group of pharmacy benefit managers can pad their own profits by driving up costs for consumers,” Weiser said. “Congress should adopt these commonsense reforms to shed light on unfair business practices and help make prescription drugs more affordable.”
A PBM is a third-party company that functions as an intermediary between insurance plans and pharmaceutical manufacturers, seemingly to reduce the cost of prescription medication for clients. It typically negotiates discounts and rebates with drug manufacturers, contracts with pharmacies, and develops and maintain drug formularies, or lists of covered drugs.
Because a PBM ultimately decides which drugs it covers, it can bargain for rebates from drug manufacturers who want to get their products on its “formularies,” or lists of covered drugs. As a result of this leverage, PBMs essentially force drug manufacturers to raise list prices to provide ever-growing rebates.
In a letter to congressional leaders, the attorneys general emphasize the urgent need for legislative action to address potential abuses within the PBM industry. Specifically, the coalition highlights three bills – the DRUG Act (S.1542/H.R. 6283), Protecting Patients Against PBM Abuses Act (H.R. 2880), and the Lower Costs, More Transparency Act (H.R. 5378) – as crucial pieces of legislation that offer necessary reforms.
The legislation is intended to limit PBMs from unjustifiably increasing drug prices and to mandate steps that increase transparency of their practices. Specifically, the proposed law would obligate PBMs to furnish pricing data to health plans and federal and state regulators in a standardized format. Such measures will empower health plans to negotiate more advantageous agreements with PBMs and enable regulators to hold PBMs accountable for their actions more effectively.
The states are seeking congressional action because PBMs routinely defy state regulatory agencies and public health plans by refusing data disclosure requests.
*************************